Diseases of the bone marrow: symptoms, diagnosis, treatment. Thrombocytopenia
Thrombocytopenia- a pathological condition characterized by a decrease in the number of platelets circulating in the peripheral blood, less than 150,000 in one microliter. This is accompanied by increased bleeding and a delayed stop of bleeding from small vessels. Thrombocytopenia may be independent blood disease, and can also be a symptom of various pathologies of other organs and systems.
The frequency of thrombocytopenia as an independent disease varies depending on the specific pathology. There are two peaks of incidence - at preschool age and after forty years. The most common is idiopathic thrombocytopenia ( 60 cases per 1 million population). The ratio of women and men in the structure of morbidity is 3:1. Among children, the frequency of this disease is slightly less ( 50 cases per 1 million).
Interesting Facts
- About 66,000 new platelets are formed in the human body per day. About the same amount is destroyed.
- Platelets play a major role in stopping bleeding from small vessels up to 100 micrometers in diameter ( primary hemostasis). Bleeding from large vessels is stopped with the participation of plasma coagulation factors ( secondary hemostasis).
- The platelet, although it belongs to the cellular elements of the blood, is not in fact a full-fledged cell.
- Clinical manifestations of thrombocytopenia develop only if the level of platelets drops by more than three times ( less than 50,000 in 1 microliter of blood).
The role of platelets in the body

For a correct understanding of the causes and mechanisms of development of this condition, certain knowledge from the field of physiology of the blood system is required.
Formation and function of platelets
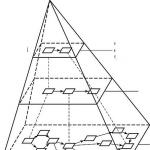
Platelets are blood cells that are flat, non-nuclear platelets measuring 1-2 micrometers ( micron), oval or rounded. In the non-activated state, they have a smooth surface. Their formation occurs in the red bone marrow from progenitor cells - megakaryocytes.
A megakaryocyte is a relatively large cell filled almost completely with cytoplasm ( internal environment of a living cell) and having long processes ( up to 120 µm). In the process of maturation, small fragments of the cytoplasm of these processes are separated from the megakaryocyte and enter the peripheral circulation - these are platelets. From 2000 to 8000 platelets are formed from each megakaryocyte.
The growth and development of megakaryocytes is controlled by a special protein hormone - thrombopoietin. Formed in the liver, kidneys and skeletal muscles, thrombopoietin is transferred by blood flow to the red bone marrow, where it stimulates the formation of megakaryocytes and platelets. An increase in the number of platelets, in turn, causes inhibition of the formation of thrombopoietin - thus their number in the blood is maintained at a certain level.
The main functions of platelets are:
- Hemostasis ( stop bleeding). When a blood vessel is damaged, platelets are immediately activated. As a result, serotonin is released from them - a biologically active substance that causes vasospasm. In addition, many processes form on the surface of activated platelets, with the help of which they are connected to the damaged vessel wall ( adhesion) and with each other ( aggregation). As a result of these reactions, a platelet plug is formed, which clogs the lumen of the vessel and stops bleeding. The described process takes 2 - 4 minutes.
- Vascular nutrition. When activated platelets are destroyed, growth factors are released that enhance the nutrition of the vascular wall and contribute to the process of its recovery after injury.
Platelet destruction
Under normal conditions, platelets circulate in the peripheral blood for 8 days, performing their functions. After this period, their structure changes, as a result of which they are captured and destroyed by the spleen, an organ involved in the exclusion of blood elements with a disturbed structure from the bloodstream ( platelets, erythrocytes and other cells).

Violation at any of the levels listed above can lead to a decrease in the number of platelets circulating in the peripheral blood.
Depending on the cause and mechanism of development, there are:
- hereditary thrombocytopenia;
- productive thrombocytopenia;
- thrombocytopenia destruction;
- consumption thrombocytopenia;
- redistribution thrombocytopenia;
- breeding thrombocytopenia.
Hereditary thrombocytopenia
This group includes diseases in which the main role belongs to genetic mutations.
Hereditary thrombocytopenias are :
- May-Hegglin anomaly;
- Wiskott-Aldrich syndrome;
- Bernard-Soulier syndrome;
- congenital amegakaryocytic thrombocytopenia;
- TAR - Syndrome.
May-Hegglin Anomaly
A rare genetic disease with an autosomal dominant pattern of inheritance ( if one of the parents is sick, then the probability of having a sick child is 50%).
It is characterized by a violation of the process of separation of platelets from megakaryocytes in the red bone marrow, resulting in a decrease in the number of formed platelets, which are gigantic in size ( 6 - 7 micrometers). In addition, with this disease, there are violations of the formation of leukocytes, which is manifested by a violation of their structure and leukopenia ( decrease in the number of leukocytes in peripheral blood).
Wiskott-Aldrich Syndrome
An inherited disease caused by genetic mutations that result in the formation of abnormal, small ( less than 1 micrometer in diameter) platelets. Due to the disturbed structure, they are excessively destroyed in the spleen, as a result of which their life span is reduced to several hours.
Also, the disease is characterized by skin eczema ( inflammation of the upper layers of the skin) and predisposition to infections ( due to immune system disorders). Only boys get sick with a frequency of 4-10 cases per 1 million.
Bernard-Soulier Syndrome
inherited autosomal recessive disorder ( appears in a child only if he inherited the defective gene from both parents) that manifests itself in early childhood. Characterized by the formation of giant ( 6 - 8 micrometers), functionally incompetent platelets. They are unable to attach to the wall of the damaged vessel and communicate with each other ( processes of adhesion and aggregation are broken) and undergo increased destruction in the spleen.
An inherited autosomal recessive disorder that manifests itself in infancy. It is characterized by mutations in the gene responsible for the sensitivity of megakaryocytes to a factor that regulates their growth and development ( thrombopoietin), as a result of which the production of platelets by the bone marrow is disrupted.
TAR - Syndrome
Rare hereditary disease 1 case per 100,000 newborns) with an autosomal recessive type of inheritance, characterized by congenital thrombocytopenia and the absence of both radius bones.
Thrombocytopenia in TAR syndrome develops as a result of a mutation of the gene responsible for the growth and development of megakaryocytes, resulting in an isolated decrease in the number of platelets in the peripheral blood.
Productive thrombocytopenia
This group includes diseases of the hematopoietic system, in which the formation of platelets in the red bone marrow is impaired.
Productive thrombocytopenia can be caused by:
- aplastic anemia;
- myelodysplastic syndrome;
- megaloblastic anemia;
- acute leukemia;
- myelofibrosis;
- cancer metastases;
- cytotoxic drugs;
- hypersensitivity to various medicines;
- radiation;
- alcohol abuse.
aplastic anemia
This pathology is characterized by inhibition of hematopoiesis in the red bone marrow, which is manifested by a decrease in peripheral blood of all types of cells - platelets ( thrombocytopenia), leukocytes ( leukopenia), erythrocytes ( anemia) and lymphocytes ( lymphopenia).
It is not always possible to establish the cause of the disease. Certain medications may be predisposing factors ( quinine, chloramphenicol), toxins ( pesticides, chemical solvents), radiation, human immunodeficiency virus ( HIV).
myelodysplastic syndrome
A group of diseases of a tumor nature, characterized by impaired hematopoiesis in the red bone marrow. With this syndrome, accelerated reproduction of hematopoietic cells is noted, but the processes of their maturation are disturbed. As a result, a large number of functionally immature blood cells ( including platelets). They are unable to perform their functions and undergo apoptosis ( self-destruction process), which is manifested by thrombocytopenia, leukopenia and anemia.
Megaloblastic anemias
This condition develops when there is a deficiency in the body of vitamin B12 and / or folic acid. With a lack of these substances, the processes of DNA formation are disrupted ( deoxyribonucleic acid), which provides storage and transmission of genetic information, as well as the processes of cellular development and functioning. In this case, first of all, tissues and organs suffer, in which the processes of cell division are most pronounced ( blood, mucous membranes).
Acute leukemia
A tumor disease of the blood system in which a mutation of the stem cell of the bone marrow occurs ( Normally, all blood cells develop from stem cells.). As a result, a rapid, uncontrolled division of this cell begins with the formation of many clones that are not able to perform specific functions. Gradually, the number of tumor clones increases and they displace hematopoietic cells from the red bone marrow, which is manifested by pancytopenia ( decrease in peripheral blood of all types of cells - platelets, erythrocytes, leukocytes and lymphocytes).
This mechanism of development of thrombocytopenia is also characteristic of other tumors of the hematopoietic system.
Myelofibrosis
A chronic disease characterized by the development of fibrous tissue in the bone marrow. The mechanism of development is similar to the tumor process - a mutation of the stem cell occurs, as a result of which the formation of fibrous tissue increases, which gradually replaces the entire substance of the bone marrow.
A distinctive feature of myelofibrosis is the development of foci of hematopoiesis in other organs - in the liver and spleen, and the size of these organs increases significantly.
Cancer metastases
Tumor diseases of various localization in the last stages of development are prone to metastasis - tumor cells leave the primary focus and spread throughout the body, settling and starting to multiply in almost any organs and tissues. This, according to the mechanism described above, can lead to the exclusion of hematopoietic cells from the red bone marrow and the development of pancytopenia.
Cytostatic drugs
This group of drugs is used to treat tumors of various origins. One of the representatives is methotrexate. Its action is due to a violation of the process of DNA synthesis in tumor cells, due to which the process of tumor growth slows down.
Adverse reactions of such drugs may be inhibition of hematopoiesis in the bone marrow with a decrease in the number of peripheral blood cells.
Hypersensitivity to various medications
As a result of individual characteristics ( most often as a result of a genetic predisposition) some people may experience hypersensitivity to drugs of various groups. These drugs can have a destructive effect directly on bone marrow megakaryocytes, disrupting the process of their maturation and the formation of platelets.
Such conditions develop relatively rarely and are not mandatory adverse reactions when using drugs.
The drugs most commonly associated with thrombocytopenia are:
- antibiotics ( chloramphenicol, sulfonamides);
- diuretics ( diuretics) (hydrochlorothiazide, furosemide);
- anticonvulsants ( phenobarbital);
- antipsychotics ( prochlorperazine, meprobamate);
- antithyroid drugs ( thiamazole);
- anti-diabetic drugs ( glibenclamide, glipizide);
- anti-inflammatory drugs ( indomethacin).
Radiation
The impact of ionizing radiation, including radiation therapy in the treatment of tumors, can have both a direct destructive effect on the hematopoietic cells of the red bone marrow, and cause mutations at various levels of hematopoiesis with the subsequent development of hemoblastoses ( tumor diseases of the hematopoietic tissue).
Alcohol abuse
Ethyl alcohol, which is the active substance of most types of alcoholic beverages, in high concentrations can have a depressing effect on the processes of hematopoiesis in the red bone marrow. At the same time, there is a decrease in the number of platelets in the blood, as well as other types of cells ( erythrocytes, leukocytes).
Most often, this condition develops with binges, when high concentrations of ethyl alcohol affect the bone marrow for a long time. The resulting thrombocytopenia, as a rule, is temporary and disappears a few days after the cessation of alcohol consumption, however, with frequent and prolonged binges, irreversible changes may develop in the bone marrow.
Thrombocytopenia destruction
In this case, the cause of the disease is the increased destruction of platelets, which occurs mainly in the spleen ( in some diseases, platelets in a smaller amount can be destroyed in the liver and in the lymph nodes or directly in the vascular bed).
Increased destruction of platelets can be observed with:
- idiopathic thrombocytopenic purpura;
- thrombocytopenia of newborns;
- post-transfusion thrombocytopenia;
- Evans-Fischer syndrome;
- taking certain medications drug thrombocytopenia);
- some viral diseases viral thrombocytopenia).
Idiopathic thrombocytopenic purpura ( AND SO ON)
Synonym - autoimmune thrombocytopenia. This disease is characterized by a decrease in the number of platelets in the peripheral blood ( the composition of other cellular elements of the blood is not disturbed) as a result of their enhanced destruction. The causes of the disease are unknown. A genetic predisposition to the development of the disease is assumed, and there is also a connection with the action of some predisposing factors.
Factors provoking the development of ITP can be:
- viral and bacterial infections;
- preventive vaccinations;
- some medicines ( furosemide, indomethacin);
- excessive insolation;
On the surface of platelets like on the surface of any cell in the body) there are certain molecular complexes called antigens. When a foreign antigen enters the body, the immune system produces specific antibodies. They interact with the antigen, leading to the destruction of the cell on the surface of which it is located.
With autoimmune thrombocytopenia, the spleen begins to produce antibodies to antigens of its own platelets. Antibodies attach to the membrane of platelets and "tag" them, as a result of which, when passing through the spleen, platelets are captured and destroyed in it ( in smaller amounts, destruction occurs in the liver and lymph nodes). Thus, the life of platelets is shortened to a few hours.
A decrease in platelets leads to increased production of thrombopoietin in the liver, which increases the rate of maturation of megakaryocytes and the formation of platelets in the red bone marrow. However, with the further development of the disease, the compensatory capabilities of the bone marrow are depleted, and thrombocytopenia develops.
Sometimes, if a pregnant woman has autoimmune thrombocytopenia, antibodies to her platelets can pass through the placental barrier and destroy normal fetal platelets.
This condition develops if there are antigens on the surface of the child's platelets that are not on the mother's platelets. In this case, antibodies class G immunoglobulins capable of crossing the placental barrier), produced in the mother's body, enter the baby's bloodstream and cause the destruction of his platelets.
Maternal antibodies can destroy fetal platelets at 20 weeks of gestation, resulting in a child already at birth with severe thrombocytopenia.
This condition develops after a blood or platelet transfusion and is characterized by severe destruction of platelets in the spleen. The mechanism of development is associated with the transfusion of foreign platelets to the patient, to which antibodies begin to be produced. It takes a certain time for the production and entry of antibodies in the blood, therefore, a decrease in platelets is noted on the 7th - 8th day after a blood transfusion.
Evans-Fischer Syndrome
This syndrome develops in some systemic diseases ( systemic lupus erythematosus, autoimmune hepatitis, rheumatoid arthritis) or without predisposing diseases against the background of relative well-being ( idiopathic form). It is characterized by the formation of antibodies to normal erythrocytes and platelets of the body, as a result of which the cells "labeled" with antibodies are destroyed in the spleen, liver and bone marrow.
Drug thrombocytopenia
Some drugs have the ability to bind to antigens on the surface of blood cells, including platelet antigens. As a result, antibodies can be produced against the formed complex, which leads to the destruction of platelets in the spleen.
The destruction of platelets begins a few days after the start of the medication. When the drug is discontinued, platelets are destroyed, on the surface of which drug antigens have already been fixed, however, newly produced platelets are not exposed to the action of antibodies, their number in the blood is gradually restored, and the manifestations of the disease disappear.
Viral thrombocytopenia
Viruses, getting into the human body, penetrate into various cells and multiply intensively in them.
The development of a virus in a living cell is characterized by:
- the appearance of viral antigens on the cell surface;
- a change in its own cellular antigens under the influence of the virus.
As a result, antibodies begin to be produced against viral or altered self antigens, which leads to the destruction of the affected cells in the spleen.
The development of thrombocytopenia can provoke:
- rubella virus;
- chickenpox virus ( chickenpox);
- measles virus;
- influenza virus.
In rare cases, the described mechanism can cause the development of thrombocytopenia during vaccination.
Thrombocytopenia consumption
This form of the disease is characterized by platelet activation directly in the vascular bed. As a result, blood coagulation mechanisms are triggered, which are often pronounced.
In response to increased consumption of platelets, their production increases. If the cause of platelet activation is not eliminated, the compensatory capabilities of the red bone marrow are depleted with the development of thrombocytopenia.
The activation of platelets in the vascular bed can be provoked by:
- disseminated intravascular coagulation syndrome;
- thrombotic thrombocytopenic purpura;
- hemolytic-uremic syndrome.
Disseminated intravascular coagulation syndrome ( DIC)
A condition that develops as a result of massive damage to tissues and internal organs, which activates the blood coagulation system, followed by its depletion.
Platelet activation in this syndrome occurs as a result of the abundant release of coagulation factors from damaged tissues. This leads to the formation of numerous blood clots in the vascular bed, which clog the gaps of small vessels, disrupting the blood supply to the brain, liver, kidneys and other organs.
As a result of impaired blood delivery to all internal organs, the anticoagulant system is activated, aimed at destroying blood clots and restoring blood flow. As a result, against the background of the depletion of platelets and other clotting factors, the blood completely loses its ability to clot. There are massive external and internal bleeding, which often ends in death.
DIC can be caused by:
- massive tissue destruction with burns, injuries, operations, transfusion of incompatible blood);
- severe infections;
- destruction of large tumors;
- chemotherapy in the treatment of tumors;
- shock of any etiology;
- organ transplant.
Thrombotic thrombocytopenic purpura ( TTP)
The basis of this disease is an insufficient amount of an anticoagulant factor, prostacyclin, in the blood. Normally, it is produced by the endothelium inner surface of blood vessels) and prevents the process of platelet activation and aggregation ( sticking them together and forming a blood clot). In TTP, impaired release of this factor leads to local activation of platelets and the formation of microthrombi, vascular damage and the development of intravascular hemolysis ( destruction of erythrocytes directly in the vascular bed).
Hemolytic uremic syndrome ( GUS)
A disease that occurs predominantly in children and is mainly due to intestinal infections ( dysentery, escherichiosis). There are also non-infectious causes of the disease ( certain medications, hereditary predisposition, systemic diseases).
With HUS caused by infection, bacterial toxins are released into the blood, damaging the vascular endothelium, which is accompanied by platelet activation, their attachment to damaged areas, followed by the formation of microthrombi and impaired microcirculation of internal organs.
Thrombocytopenia redistribution
Under normal conditions, about 30% of platelets are deposited ( postponed) in the spleen. If necessary, they are released into the circulating blood.
Some diseases can lead to splenomegaly ( enlargement of the spleen), as a result of which up to 90% of all platelets in the body can be retained in it. Since regulatory systems control the total number of platelets in the body, and not their concentration in the circulating blood, the retention of platelets in an enlarged spleen does not cause a compensatory increase in their production.
Splenomegaly can be caused by:
- cirrhosis of the liver;
- infections ( hepatitis, tuberculosis, malaria);
- systemic lupus erythematosus;
- tumors of the blood system leukemia, lymphoma);
With a long course of the disease, platelets retained in the spleen can undergo massive destruction, followed by the development of compensatory reactions in the bone marrow.
Thrombocytopenia of redistribution can develop with hemangioma - a benign tumor consisting of vascular cells. It has been scientifically proven that platelet sequestration occurs in such neoplasms ( delay and shutdown of them from circulation with possible subsequent destruction). This fact is confirmed by the disappearance of thrombocytopenia after surgical removal of the hemangioma.
Thrombocytopenia breeding
This condition develops in patients who are in the hospital ( more common after massive blood loss), which are transfused with large volumes of liquids, plasma and plasma substitutes, erythrocyte mass, without compensating for the loss of platelets. As a result, their concentration in the blood can decrease so much that even the release of platelets from the depot is not able to maintain the normal functioning of the coagulation system.
Symptoms of thrombocytopenia

Since the function of platelets is hemostasis ( stop bleeding), then the main manifestations of their deficiency in the body will be bleeding of various localization and intensity. Clinically, thrombocytopenia is not expressed in any way, while the concentration of platelets exceeds 50,000 in one microliter of blood, and only with a further decrease in their number do symptoms of the disease begin to appear.
Dangerous is the fact that even at lower platelet concentrations, a person does not experience a significant deterioration in the general condition and feels comfortable, despite the risk of developing life-threatening conditions ( severe anemia, cerebral hemorrhage).
The mechanism of development of all symptoms of thrombocytopenia is the same - a decrease in the concentration of platelets leads to malnutrition of the walls of small vessels ( mostly capillaries) and their increased fragility. As a result, spontaneously or under the influence of a physical factor of minimal intensity, the integrity of the capillaries is broken and bleeding develops.
Since the number of platelets is reduced, a platelet plug does not form in damaged vessels, which causes a massive outflow of blood from the circulatory bed into the surrounding tissues.
The symptoms of thrombocytopenia are:
- Hemorrhages in the skin and mucous membranes ( purpura). They appear as small red spots, especially pronounced in places of compression and friction by clothing, and are formed as a result of soaking the skin and mucous membranes with blood. The spots are painless, do not protrude above the surface of the skin and do not disappear when pressed. May be observed as single pinpoint hemorrhages ( petechiae) and large in size ( ecchymosis - more than 3 mm in diameter, bruising - a few centimeters in diameter). At the same time, bruises of various colors can be observed - red and blue ( earlier) or greenish and yellow ( later).
- Frequent nosebleeds. The mucous membrane of the nose is abundantly supplied with blood and contains a large number of capillaries. Their increased fragility, which occurs due to a decrease in the concentration of platelets, leads to profuse bleeding from the nose. Sneezing, colds, microtrauma ( when picking your nose), ingress of a foreign body. The blood that flows out is bright red. The duration of bleeding can exceed tens of minutes, as a result of which a person loses up to several hundred milliliters of blood.
- Bleeding gums. Many people may experience some bleeding gums when brushing their teeth. With thrombocytopenia, this phenomenon is especially pronounced, bleeding develops on a large surface of the gums and continues for a long time.
- Gastrointestinal bleeding. They arise as a result of increased fragility of the vessels of the mucous membrane of the gastrointestinal system, as well as when it is injured by rough, hard food. As a result, blood can pass out with feces ( melena), staining it red, or with vomit ( hematemesis), which is more typical for bleeding from the gastric mucosa. Blood loss sometimes reaches hundreds of milliliters of blood, which can threaten a person's life.
- Appearance of blood in urine hematuria). This phenomenon can be observed with hemorrhages in the mucous membranes of the bladder and urinary tract. At the same time, depending on the volume of blood loss, urine may acquire a bright red color ( gross hematuria), or the presence of blood in the urine will be determined only by microscopic examination ( microhematuria).
- Prolonged profuse menstruation. Under normal conditions, menstrual bleeding lasts about 3 to 5 days. The total volume of secretions during this period does not exceed 150 ml, including the sloughing layer of the endometrium. The amount of blood lost does not exceed 50 - 80 ml. Thrombocytopenia is associated with profuse bleeding over 150 ml) during menstruation ( hypermenorrhea), as well as on other days of the menstrual cycle.
- Prolonged bleeding during tooth extraction. Tooth extraction is associated with rupture of the dental artery and damage to the capillaries of the gums. Under normal conditions, within 5 - 20 minutes, the place where the tooth used to be ( alveolar process of the jaw), is filled with a blood clot, and bleeding stops. With a decrease in the number of platelets in the blood, the formation of this clot is disrupted, bleeding from damaged capillaries does not stop and can continue for a long time.
Very often, the clinical picture of thrombocytopenia is supplemented by the symptoms of the diseases that led to its occurrence - they must also be taken into account in the diagnostic process.
Diagnosis of the causes of thrombocytopenia
 In most cases, a decrease in the number of platelets is a symptom of a certain disease or pathological condition. Establishing the cause and mechanism of development of thrombocytopenia allows you to make a more accurate diagnosis and prescribe appropriate treatment.
In most cases, a decrease in the number of platelets is a symptom of a certain disease or pathological condition. Establishing the cause and mechanism of development of thrombocytopenia allows you to make a more accurate diagnosis and prescribe appropriate treatment.
In the diagnosis of thrombocytopenia and its causes, the following are used:
- General blood analysis ( UAC). Allows you to determine the quantitative composition of the blood, as well as to study the shape and size of individual cells.
- according to Duke). Allows you to evaluate the functional state of platelets and the blood coagulation caused by them.
- Determination of blood clotting time. Measures the time it takes for blood from a vein to clot ( blood will start to clot). This method allows to identify violations of secondary hemostasis, which may accompany thrombocytopenia in some diseases.
- Puncture of the red bone marrow. The essence of the method is to pierce certain bones of the body ( sternum) with a special sterile needle and taking 10-20 ml of bone marrow substance. Smears are prepared from the material obtained and examined under a microscope. This method provides information about the state of hematopoiesis, as well as quantitative or qualitative changes in hematopoietic cells.
- Determination of antibodies in the blood. A highly accurate method that allows you to determine the presence of antibodies to platelets, as well as to other cells of the body, to viruses or medicines.
- Genetic research. It is carried out with suspicion of hereditary thrombocytopenia. Allows you to identify gene mutations in the parents and next of kin of the patient.
- Ultrasonography. A method for studying the structure and density of internal organs using the phenomenon of reflection of sound waves from tissues of various densities. Allows you to determine the size of the spleen, liver, suspect tumors of various organs.
- Magnetic resonance imaging ( MRI). A modern high-precision method that allows you to get a layered image of the structure of internal organs and blood vessels.
Diagnosis of thrombocytopenia
Minor thrombocytopenia may be detected incidentally on a complete blood count. At a platelet concentration below 50,000 in one microliter, clinical manifestations of the disease may develop, which causes a visit to a doctor. In such cases, additional methods are used to confirm the diagnosis.
In the laboratory diagnosis of thrombocytopenia, the following are used:
- general blood analysis;
- determination of bleeding time ( Duke test).
General blood analysis
The simplest and at the same time the most informative laboratory research method that allows you to accurately determine the concentration of platelets in the blood.
Blood sampling for analysis is carried out in the morning, on an empty stomach. The skin on the palmar surface of the finger usually nameless) are treated with cotton wool soaked in an alcohol solution, after which they are pierced with a disposable lancet ( thin and sharp double-sided blade) to a depth of 2 - 4 mm. The first drop of blood that appears is removed with a cotton swab. Then, with a sterile pipette, blood is collected for analysis ( usually 1 - 3 milliliters).
Blood is examined in a special device - a hematological analyzer, which quickly and accurately calculates the quantitative composition of all blood cells. The data obtained make it possible to detect a decrease in the number of platelets, and may also indicate quantitative changes in other blood cells, which contributes to the diagnosis of the cause of the disease.
Another way is to examine a blood smear under a microscope, which allows you to count the number of blood cells, as well as visually assess their size and structure.
Determination of bleeding time ( Duke test)
This method allows you to visually assess the rate of stopping bleeding from small vessels ( capillaries), which characterizes the hemostatic ( hemostatic) platelet function.
The essence of the method is as follows - with a disposable lancet or a needle from a syringe, they pierce the skin of the tip of the ring finger to a depth of 3-4 millimeters and turn on the stopwatch. In the future, every 10 seconds, a drop of blood is removed with a sterile napkin, without touching the skin in the injection area.
Normally, bleeding should stop after 2 to 4 minutes. An increase in bleeding time indicates a decrease in the number of platelets or their functional failure and requires additional research.
Diagnosis of hereditary thrombocytopenia
This group of diseases is characterized by development in early childhood. Genetic research allows to identify a defective gene in parents, which is characteristic for each individual disease.
Diagnostic criteria for hereditary thrombocytopenia
| Name of the disease | Diagnostic criteria |
| May-Hegglin Anomaly |
|
| Wiskott-Aldrich Syndrome |
|
| Bernard-Soulier Syndrome |
|
| Congenital amegakaryocytic thrombocytopenia |
|
| TAR - Syndrome |
|
Diagnosis of productive thrombocytopenia
In diseases from this group, in addition to reduced production of platelets, there is almost always a violation of the formation of other blood cells with characteristic clinical and laboratory manifestations.
Diagnostic criteria for productive thrombocytopenia
| Cause of thrombocytopenia | Diagnostic criteria |
| aplastic anemia |
|
| myelodysplastic syndrome |
|
| Megaloblastic anemias |
|
| Acute leukemia |
|
| Myelofibrosis |
|
| Cancer metastases |
|
| Cytostatic drugs |
|
| Hypersensitivity to medications |
|
| Radiation |
|
| Alcohol abuse |
|
Diagnosis of thrombocytopenia destruction
The destruction of platelets in these conditions occurs mainly in the spleen. A decrease in the number of platelets in the peripheral blood causes a compensatory increase in their production, which is confirmed by bone marrow puncture ( punctate shows an increase in the number of megakaryocytes).
Diagnostic criteria for thrombocytopenia destruction
| Cause of thrombocytopenia | Diagnostic criteria |
| Idiopathic thrombocytopenic purpura |
|
| Thrombocytopenia of the newborn |
|
| Post-transfusion thrombocytopenia |
|
| Evans-Fischer Syndrome |
|
| Drug thrombocytopenia |
|
| Viral thrombocytopenia |
|
Diagnosis of consumption thrombocytopenia
A characteristic feature of some diseases from this group is the diversity of indicators of the cellular composition of the blood and the functions of the coagulation system in different periods of the disease.
So, during the development of DIC, when there is an increased activation of platelets in the vascular bed, their number in a general blood test may be normal or even increased. In the later stages, when the body's coagulation system is depleted, thrombocytopenia and other blood clotting disorders can be determined in the blood.
Diagnostic criteria for consumption thrombocytopenia
| Cause of thrombocytopenia | Diagnostic criteria | |
| DIC | At the onset of the disease | At the end of the disease |
|
|
|
| Thrombotic thrombocytopenic purpura |
|
|
| Hemolytic uremic syndrome |
|
|
Diagnosis of Thrombocytopenia Redistribution
Diagnostic difficulties in this disease, as a rule, do not arise. In the clinical picture, manifestations of the underlying disease come to the fore, and laboratory and instrumental methods are used to confirm the diagnosis.
Diagnostic criteria for redistribution thrombocytopenia are:
- Ultrasonography. Allows you to set the exact size of the enlarged spleen. An increase in the size and change in the structure of the liver can also be detected ( with cirrhosis).
- Changes in the UAC. In the blood, thrombocytopenia of varying degrees of intensity is noted. Microscopic examination of a blood smear reveals normal or slightly reduced platelets in size. With a long course of the disease, anemia, leukopenia, up to pancytopenia may appear ( due to the destruction of all types of blood cells by the spleen).
- Determination of antibodies in the blood. Antibodies to various bacteria, antinuclear antibodies ( with systemic lupus erythematosus).
- Puncture of the bone marrow. At the onset of the disease, no changes in the bone marrow are observed. If the process of massive destruction of platelets in the spleen begins, then in the bone marrow there is an increased formation of megakaryocytes and other hematopoietic cells.
Diagnosis of dilutional thrombocytopenia
Diagnosis of this condition does not cause difficulties. In the history of the disease, as a rule, massive blood loss is noted, followed by the transfusion of large volumes of fluid or plasma.
From laboratory analyzes is carried out:
- General blood analysis. Thrombocytopenia is determined, anemia is possible ( with loss and insufficient replenishment of the number of red blood cells).
- Microscopic examination of a blood smear. Individual platelets of normal size and shape are determined, located at a relatively large distance from each other.
Additional laboratory and instrumental studies, as a rule, are not required.
Treatment of thrombocytopenia
 Treatment of thrombocytopenia should be prescribed by a hematologist after a thorough examination of the patient.
Treatment of thrombocytopenia should be prescribed by a hematologist after a thorough examination of the patient.
What is the severity of the condition of patients with thrombocytopenia?
The decision on the need for specific treatment is made depending on the severity of the disease, which is determined by the level of platelets in the blood and the severity of the manifestations of the hemorrhagic syndrome ( bleeding).
Thrombocytopenia may be:
- Light severity. The concentration of platelets is from 50 to 150 thousand in one microliter of blood. This amount is sufficient to maintain the normal state of the walls of the capillaries and prevent the release of blood from the vascular bed. Bleeding with mild thrombocytopenia does not develop. Medical treatment is usually not required. Expectant management and determination of the cause of the decrease in platelets is recommended.
- Medium severity. The concentration of platelets is from 20 to 50 thousand in one microliter of blood. Perhaps the appearance of hemorrhages in the mucous membrane of the mouth, increased bleeding of the gums, increased nosebleeds. With bruises and injuries, extensive hemorrhages can form in the skin that do not correspond to the amount of damage. Medical therapy is recommended only if there are factors that increase the risk of bleeding ( ulcers of the gastrointestinal system, professional activities or sports associated with frequent injuries).
- Severe degree. The concentration of platelets in the blood is below 20 thousand in one microliter. Spontaneous, profuse hemorrhages in the skin, mucous membranes of the mouth, frequent and profuse nosebleeds and other manifestations of hemorrhagic syndrome are characteristic. The general condition, as a rule, does not correspond to the severity of laboratory data - patients feel comfortable and complain only of a cosmetic defect as a result of skin hemorrhages.
Is hospitalization necessary for the treatment of thrombocytopenia?
Patients with mild thrombocytopenia usually do not need hospitalization or any treatment. However, it is highly recommended to consult a hematologist and undergo a comprehensive examination to identify the cause of the decrease in platelet count.
With moderate thrombocytopenia without pronounced manifestations of hemorrhagic syndrome, home treatment is prescribed. Patients are informed about the nature of their disease, the risks of bleeding from injuries and the possible consequences. They are advised to limit their active lifestyle for the period of treatment and take all medications prescribed by the hematologist.
All patients with a platelet count below 20,000 in one microliter of blood are subject to mandatory hospitalization, as this is a life-threatening condition and requires immediate treatment under the constant supervision of medical personnel.
All patients with profuse hemorrhages in the face, oral mucosa, profuse nosebleeds, regardless of the level of platelets in the blood, must be hospitalized without fail. The severity of these symptoms indicates an unfavorable course of the disease and possible cerebral hemorrhage.
Medical treatment
Drug therapy is most commonly used to treat immune thrombocytopenias due to the formation of antiplatelet antibodies with subsequent destruction of platelets in the spleen.
The goals of medical treatment are:
- elimination of hemorrhagic syndrome;
- elimination of the immediate cause of thrombocytopenia;
- treatment of the disease that caused thrombocytopenia.
Medicines used in the treatment of thrombocytopenia
| Name of medication | Indications for use | Mechanism of therapeutic action | Dosage and administration |
| Prednisolone | Autoimmune thrombocytopenia, as well as secondary thrombocytopenia with the formation of antibodies to platelets. |
| The initial daily dose is 40 - 60 mg, divided into 2 - 3 doses. If necessary, the dose is increased by 5 mg per day. The course of treatment is 1 month. Upon reaching remission normalization of the number of platelets in the blood) the drug is canceled gradually, reducing the dose by 2.5 mg per week. |
| Intravenous immunoglobulin (synonyms - Intraglobin, Imbiogam) |
| The recommended dose is 400 milligrams per kilogram of body weight, once a day. The duration of treatment is 5 days. | |
| Vincristine | Same as prednisone. |
| It is used at high concentrations of antiplatelet antibodies in the blood, with the ineffectiveness of other drugs. It is administered intravenously, once a week, at a dose of 0.02 milligrams per kilogram of body weight. The course of treatment is 4 weeks. |
| Eltrombopag (synonym - Revolade) | Reducing the risk of bleeding in idiopathic thrombocytopenia. |
| Take orally in the form of tablets. The initial dose is 50 mg 1 time per day. In the absence of effect, the dose can be increased to 75 mg per day. |
| Depo Provera | Women for the prevention of blood loss during heavy menstrual bleeding caused by thrombocytopenia. |
| Every three months, a single dose of 150 milligrams is administered intramuscularly. |
| Etamzilat | Thrombocytopenia of any etiology ( except for the initial stage of DIC). |
| Take orally, 500 mg three times a day, after meals. |
| VitaminB12( synonym - cyanocobalamin) | Thrombocytopenia in megaloblastic anemia. |
| Take orally, 300 micrograms per day, one-time. |
Non-drug treatment
It includes various therapeutic and surgical measures aimed at eliminating thrombocytopenia and its causes.
Additional treatments for thrombocytopenia are:
- transfusion therapy. This method consists in the transfusion of donated blood, plasma or platelets to the patient ( depending on the existing violations of the cellular composition of the blood). This procedure can be accompanied by a number of dangerous side effects ( from infection to anaphylactic shock with fatal outcome), in connection with which it is prescribed only in life-threatening situations ( DIC, risk of cerebral hemorrhage). Blood transfusion is carried out only in a hospital under the constant supervision of a doctor.
- Splenectomy. Since the spleen is the main source of antibodies in immune thrombocytopenia, as well as the main site of platelet destruction in various diseases, its surgical removal can be a radical method of treatment ( splenectomy). Indications for surgery are the ineffectiveness of drug therapy for at least one year or recurrence of thrombocytopenia after drug withdrawal. In a large number of patients after splenectomy, there is a normalization of the number of platelets in the blood and the disappearance of the clinical manifestations of the disease.
- Bone marrow transplantation. It is an effective method for the treatment of various diseases accompanied by a decrease in platelet production in the bone marrow. Previously, the patient is prescribed large doses of cytostatics ( anticancer drugs) and drugs that suppress the immune system. The purpose of this therapy is to prevent the development of an immune response in response to the introduction of donor bone marrow, as well as the complete destruction of tumor cells in hemoblastoses ( tumors of the hematopoietic system).
Nutrition for thrombocytopenia
There is no specific diet specifically for thrombocytopenia. However, there are a number of recommendations that should be followed in order to prevent complications of the disease.
Nutrition should be complete and balanced, contain a sufficient amount of proteins, fats, carbohydrates, vitamins and minerals.
The food taken should be well processed ( crushed), so as not to injure the oral mucosa and the gastrointestinal system. It is not recommended to take rough, solid food, especially during periods of exacerbation of the disease, as this can lead to the development of gastrointestinal bleeding. You should also refrain from drinking cold and hot drinks and foods.
Alcohol should be completely excluded, as it has a direct inhibitory effect on the red bone marrow.
Consequences of thrombocytopenia
 The main manifestations of thrombocytopenia are hemorrhages and bleeding. Depending on their localization and intensity, various complications can develop, sometimes life-threatening.
The main manifestations of thrombocytopenia are hemorrhages and bleeding. Depending on their localization and intensity, various complications can develop, sometimes life-threatening.
The most formidable complications of thrombocytopenia are:
- Hemorrhage in the retina. It is one of the most dangerous manifestations of thrombocytopenia and is characterized by impregnation of the retina with blood released from damaged capillaries. The first sign of a retinal hemorrhage is a deterioration in visual acuity, after which a sensation of a spot in the eye may appear. This condition requires urgent qualified medical care, as it can lead to complete and irreversible loss of vision.
- Hemorrhage in the brain. It is a relatively rare, but the most formidable manifestation of thrombocytopenia. May occur spontaneously or with head trauma. The onset of this condition is usually preceded by other symptoms of the disease ( hemorrhages in the mucous membrane of the mouth and in the skin of the face, nosebleeds). Manifestations depend on the site of the hemorrhage and the amount of blood that has flowed out. The prognosis is poor - about a quarter of cases are fatal.
- Posthemorrhagic anemia. Most often it develops with heavy bleeding in the gastrointestinal system. It is not always possible to diagnose them immediately, and due to increased fragility of capillaries and a reduced number of platelets, bleeding can last for several hours and often recur ( are repeated). Clinically, anemia is manifested by pallor of the skin, general weakness, dizziness, and if more than 2 liters of blood are lost, death can occur.
The prognosis for thrombocytopenia is determined :
- severity and duration of the disease;
- the adequacy and timeliness of the treatment;
- presence of complications
- underlying disease causing thrombocytopenia.
All patients who have had thrombocytopenia at least once in their lives are recommended periodically ( once every 6 months) to take a general blood test for preventive purposes.
There are the following causes of acquired aplastic anemia:
- ionizing radiation;
- medications ( decaris, analgin, levomycetin, tetracycline, butadione, etc.);
- chemical compounds ( pesticides, benzene);
- diseases ( viral hepatitis A, B and C, Epstein-Barr virus, cytomegalovirus, herpes virus, HIV, parvovirus B19, etc.).
- hormonal disorders from the ovaries, thyroid gland and thymus gland.
Some harmful agents directly affect the bone marrow ( ionizing radiation, chemical and medicinal substances). Others act indirectly through autoimmune mechanisms ( viral hepatitis B).
The mechanism of development of aplastic anemia
 Today in the scientific world there are several theories describing the mechanism of development of aplastic anemia. Interestingly, all theories are fully proven, and, nevertheless, can not always explain the oppression of the bone marrow in a particular case.
Today in the scientific world there are several theories describing the mechanism of development of aplastic anemia. Interestingly, all theories are fully proven, and, nevertheless, can not always explain the oppression of the bone marrow in a particular case. There are the following theories of the pathogenesis of aplastic anemia:
- stromal;
- autoimmune;
- premature apoptosis.
Stromal theory
It has been proven that the growth and maturation of bone marrow cells is impossible without the influence of factors produced by the stroma. The stroma is an accumulation of connective tissue cells that form a kind of "skeleton" or "bed" in which bone marrow cells lie. The stroma produces substances such as IL ( interleukins) 1, 3 and 6 and stem cell factor. These substances direct the development of progenitor cells in one direction or another at various stages of their development.In 15-20% of cases of aplastic anemia, the cause of their development is insufficient formation and release of stromal growth factors. For this reason, the differentiation of blood cells stops at a certain stage of development. In the bone marrow, a special study can detect an accumulation of precursors of blood cells. In the peripheral blood, there is an increase in erythropoietin, which normally affects the stroma of the bone marrow.
autoimmune theory
In bone marrow biopsies, in most cases, foci of accumulation of T-killer cells, monocytes, tumor necrosis factor alpha and interferon gamma are found, indicating an inflammatory mechanism for the development of aplastic anemia. A more detailed study of the cells of bone marrow sprouts revealed the absence of a certain protein-carbohydrate complex encoded by the PIG-A gene on their surface. Mutation of this gene leads to the absence of the synthesis of the above complex. As a result, there is no inactivation of the complement system, one of the links in the body's immune defense. As a result, the immune system perceives its own cells as foreign and seeks to destroy them. The larger the population of mutated cells in relation to healthy ones, the more pronounced is the violation of the synthesis of bone marrow cells.Theory of premature apoptosis
Apoptosis is a physiological process in which there is an independent destruction of cells with certain mutational anomalies or cells that have outlived their allotted time. Through apoptosis, the body is protected from the accumulation of mutations and the resulting complications, predominantly of tumor origin. However, apoptosis can also become a pathological process, when it leads to premature self-destruction of cells. The cause of premature apoptosis is a mutation in the gene that synthesizes the P-450 protein.Despite the existence of several successful theories of the development of aplastic anemia, numerous studies in this direction are still being conducted in the scientific world. However, for a practitioner, and even more so for a patient, the search for a mechanism by which the development of the disease occurs almost never makes sense. This is due to the fact that today there are no more or less effective drugs, in addition to steroid hormones, that can slow down the progression of anemia or at least partially compensate for it. In addition, the most effective treatment today is bone marrow transplantation. Therefore, the study of the mechanism of development of aplastic anemia is of exclusively scientific interest.
Symptoms of aplastic anemia
 The classic symptoms of aplastic anemia fit into the following syndromes:
The classic symptoms of aplastic anemia fit into the following syndromes:
- anemic;
- hemorrhagic;
- toxic-infectious.
- mixed shortness of breath that occurs with moderate and slight physical exertion;
- increased fatigue;
- darkening and flies before the eyes;
- dizziness;
- the appearance of systolic anemic heart murmurs, etc.
- slow stop bleeding;
- frequent nosebleeds;
- profuse menstruation;
- skin bruising;
- thrombocytopenic purpura;
- easy bruising, etc.
- weak immune status of the body;
- severe course of mild viral diseases;
- slow healing of wounds;
- suppuration of scratches, etc.
Anemia Fanconi
A rare, severe congenital aplastic anemia diagnosed between the ages of 4 and 10 years. It affects the male and female gender with equal frequency. It develops due to the high susceptibility of the DNA of body cells, and bone marrow in particular, to various kinds of mutations. Clinically manifested by the above three syndromes. The severity of the symptoms of the disease has a wave-like character with periods of remissions and exacerbations. There is a high risk of developing malignant tumor processes.Up to 80% of patients are born with the following bodily anomalies:
- From the musculoskeletal system - additional, missing or fused fingers, underdevelopment or absence of shoulder blades, non-closure of the hard palate ( cleft palate, cleft lip), absence of auricles, deformation of the cartilage of the nose, additional vertebrae, scoliosis, etc.
- From the side of the nervous system - microencephaly or anencephaly, macrocephaly, spinal hernias, blindness, deafness, myasthenia gravis, paraparesis and tetraparesis, mental retardation.
- From the genitourinary system - underdevelopment or absence of kidneys, accessory kidneys, renal polycystic, S-shaped kidney, horseshoe kidney ( fusion of one of the poles) ectopia of the ureters, exstrophy ( eversion) bladder, agenesis ( lack of development) uterus, bicornuate uterus, complete infection of the hymen, anorchia ( absence of testicles), agenesis of the urethra and penis, etc.
- From the side of the cardiovascular system - non-closure of the foramen ovale and interatrial septum, open batal duct, aortic stenosis at various levels, inversion of the main vessels of the heart, etc.
- From the digestive system - stenosis and aneurysm of the intestine, diverticulosis, intestinal atresia ( blindly ending bowel), bronchoesophageal fistulas at various levels.
75% of patients have café-au-lait skin. There are also vitiligo - areas of the skin with increased or decreased pigmentation. The only way to keep the patient alive is to transfuse the missing blood components. For this reason, after 4-5 years of the disease, the skin of patients acquires a grayish tint due to excess iron during the destruction of red blood cells. In cases where congenital anomalies are compatible with life, bone marrow transplantation is allowed as a treatment. However, the prognosis of the disease is poor. Most patients die at an average age of 7 years.
Diamond-Blackfan anemia
This type of anemia is considered to be partially plastic, since it is manifested by the suppression of exclusively the erythrocyte sprout of the bone marrow without the involvement of the leukocyte and platelet sprouts. The disease is familial and can occur if at least one parent is sick with it. Since the disease is autosomal dominant, the probability of manifestation varies between 50 - 100%, depending on the combination of parental genes.The immediate cause of the disease is the low sensitivity of bone marrow cells to erythropoietin. Clinically, only anemic syndrome is observed. A high probability of developing acute leukemia has been noted. In most cases, antibodies to erythrokaryocytes are determined, so immunosuppressive treatment is often effective. Supportive care is provided through regular red blood cell transfusions.
Diagnosis of aplastic anemia
 The clinical picture of the disease can largely guide the doctor in the direction of anemia, but the diagnosis must be confirmed or refuted using laboratory tests and paraclinical studies.
The clinical picture of the disease can largely guide the doctor in the direction of anemia, but the diagnosis must be confirmed or refuted using laboratory tests and paraclinical studies. The most valuable additional studies are:
- general blood analysis ( UAC);
- blood chemistry ( TANK);
- sternal puncture;
- trepanobiopsy.
General blood analysis
Data from a complete blood count in aplastic anemia testify in favor of pancytopenia ( a decrease in the number of all three types of bone marrow cells). A decrease in the number of leukocytes is observed mainly due to a decrease in granulocytes ( neutrophils, eosinophils and basophils). Thus, the percentage of lymphocytes and monocytes in the leukocyte formula increases relatively. At various stages of the disease, inflammatory signs can be detected to some extent.Indicative indicators of KLA in aplastic anemia are:
- Hemoglobin ( Hb) – less than 110 g/l ( norm 120 – 160 g/l). Reduction due to a decrease in the number of red blood cells.
- red blood cells- 0.7 - 2.5 x 10 12 \l ( norm 3.7 x 10 12 \l). Decrease in the number of mature erythrocytes.
- Reticulocytes- less than 0.2% ( norm 0.3 - 2.0%). Decrease in the number of young forms of erythrocytes.
- color indicator – 0,85 – 1,05 (norm 0.85 - 1.05) indicates the normochromic nature of anemia ( the content of hemoglobin in the erythrocyte is within the normal range).
- Hematocrit ( ht) – less than 30 ( the norm is 35 - 42 for women and 40 - 46 for men). The ratio of the cellular composition of blood to its liquid part. There is a clear decrease in the proportion of cells in the peripheral blood.
- platelets- less than 35 ppm or 100 x 10 9 \l. Decreased platelet count.
- Leukocytes- 0.5 - 2.5 x 10 9 \l ( norm 4 - 9 x 10 9 \ l). Severe leukopenia due to a decrease in the number of granulocytes ( neutrophils, eosinophils and basophils).
- stab neutrophils – 0 – 2% (norm less than 6%). Decreased production of young forms of leukocytes.
- segmented neutrophils – 0 – 40% (norm 47 - 72%). Reducing the number of mature forms of neutrophils.
- Myelocytes – 0 – 2% (normally absent). Under conditions of granulocytopenia and layering of bacterial infection, a more pronounced than usual shift of the leukocyte formula to the left with the appearance of leukopoiesis precursor cells is observed.
- Eosinophils – 0 – 1% (norm 1 - 5%). Decrease in the number of eosinophils.
- Basophils – 0% (norm 0 – 1%). Single or complete absence of basophils.
- Lymphocytes– more than 40% ( norm 19 - 37%). The numerical number of lymphocytes remains normal. Due to the decrease in the fraction of granulocytes, relative lymphocytosis is observed ( an increase in the proportion of lymphocytes in the blood). Extremely pronounced lymphocytosis can be observed with the layering of viral infections.
- Monocytes– more than 8% ( norm 6 - 8%). The number of monocytes is unchanged and within the normal range. Monocytosis ( an increase in the proportion of monocytes in the blood) is explained by a decrease in the percentage of granulocytes in the leukocyte formula.
- Erythrocyte sedimentation rate– more than 15 – 20 mm/hour ( the norm is up to 10 mm / hour in men and up to 15 mm / hour in women). This indicator reflects the severity of the inflammatory response in the body.
- Anisocytosis- the presence of red blood cells of various sizes in the blood.
- Poikilocytosis- the presence in the blood of erythrocytes of various shapes.
Blood chemistry
Some types of biochemical blood tests can focus the doctor's attention on abnormalities in the body that indirectly fit into the three anemic syndromes listed above.Indicative indicators of the LHC in aplastic anemia are:
- Serum iron more than 30 µmol/l ( norm 9 - 30 µmol/l). An increase in serum iron due to frequent blood transfusions. High risk of developing hemochromatosis.
- Erythropoietin more than 30 IU/l ( the norm is 8 - 30 IU / l in women and 9 - 28 IU / l in men). The increase in erythropoietin occurs for two reasons. Firstly, it is not consumed by the cells of the erythrocyte germ. Secondly, its synthesis increases compensatory in response to anemia.
- HBs-AG and anti-HBcor immunoglobulins G are positive ( normal - negative). This analysis indicates the presence of viral hepatitis B. In some cases, this virus provokes the development of an autoimmune reaction against bone marrow cells.
- C-reactive protein– more than 10 – 15 mg/l ( norm 0 - 5 mg / l). It is detected during an inflammatory reaction against the background of a weakened immune system.
- Thymol test– more than 4 ( norm 0 - 4). Reveals signs of inflammation in weakened immunity.
Sternal puncture
This type of study is used to visualize bone marrow cells and their percentage. The puncture is carried out in the treatment room using sterile instruments and painkillers, mainly inhalation. The puncture site is treated alternately with several antiseptic solutions. The patient is in the supine position. For puncture, special wide needles with an insertion depth limiter are used. The syringe and plunger must provide sufficient compression, so it is preferable to use glass syringes with an iron plunger. Classically, the puncture is carried out in the body of the sternum at the level of 2-3 ribs with slow rotational movements until a sensation of failure. A sharp perforation increases the risk of the needle slipping from the sternum and injuring the organs of the chest cavity. After feeling the failure, the needle is fixed with one hand, and the syringe rod is traction with the other hand. The punctate is taken up to the mark of 0.3 - 0.5 mm, after which the needle is removed, and the hole is sealed with adhesive tape. In the absence of punctate at the puncture site, the puncture is repeated a few centimeters lower. After the puncture, the patient should continue to be in a horizontal position under the supervision of medical personnel for another 30 minutes.After removing the syringe, it is emptied onto several slides, from which 10-15 smears will subsequently be made. The smears are fixed, stained and examined according to the appropriate techniques. The result of the study is called a myelogram. The myelogram reflects the actual and relative cellular composition of the bone marrow.
With aplastic anemia, the myelogram will be poor, the number of cellular elements is significantly reduced. Cambial cells of the erythrocyte and leukocyte series are single or absent. Megakaryoblasts are absent. In rare cases, during puncture, it happens to meet grouped foci of increased cell proliferation as a compensatory response of a healthy bone marrow to anemia. Such a myelogram can be confusing because it would be indicative of the absence of aplastic anemia and therefore be a false negative.
Trepanobiopsy
Trepanobiopsy is a method of removing a piece of bone marrow from a patient's iliac wing. The advantage of this procedure over sternal puncture is that more material can be taken while maintaining its structure. A larger amount of material reduces the likelihood of a false-negative result of aplastic anemia, and the study of the structure of the bone marrow allows, in addition to cytological examination ( myelograms) to conduct a histological examination.During a trepanobiopsy, the patient is in the supine position. The needles for this procedure are similar to the needles for sternal puncture, but larger in size. Anesthesia and the material sampling technique are identical to those described above. The results of trepanobiopsy repeat the results of sternal puncture. In addition to this, an increase in the percentage of stroma in relation to hematopoietic cells is determined, as well as an increase in the proportion of yellow inactive bone marrow in relation to red active.
With the help of a blood test and the results of a trepanobiopsy, it is possible to determine the severity of aplastic anemia.
Aplastic anemia of moderate severity is determined by the following indicators:
- granulocytes less than 2.0 x 109/l;
- platelets less than 100 x 109/l;
- reticulocytes less than 2 - 3%;
- bone marrow hypoplasia on trephine biopsy.
- granulocytes less than 0.5 x 109/l;
- platelets less than 20 x 109/l;
- reticulocytes less than 1%;
- granulocytes less than 0.2 x 109/l;
- platelets are single or absent;
- reticulocytes are single or absent;
- bone marrow aplasia on trepanobiopsy.
Treatment of aplastic anemia with medicines
 Treatment of aplastic anemia is a complex and complex process. In the initial stages of the disease, various courses of therapy with glucocorticoid hormones and cytostatics are used to reduce the body's immune reactivity. In most cases, this approach gives temporary positive results, since the mechanism of development of aplastic anemia is largely associated with autoimmune reactions.
Treatment of aplastic anemia is a complex and complex process. In the initial stages of the disease, various courses of therapy with glucocorticoid hormones and cytostatics are used to reduce the body's immune reactivity. In most cases, this approach gives temporary positive results, since the mechanism of development of aplastic anemia is largely associated with autoimmune reactions. Medications are an integral part of the treatment of aplastic anemia. The three most commonly used drugs are immunosuppressants ( ), cytostatics ( cyclophosphamide, 6-mercaptopuril, cyclosporine A, methotrexate, imuran, etc.) and antibiotics ( cephalosporins, macrolides, azalides, chlorquinolones, etc.). Less commonly, drugs can be used to correct blood pressure, disorders of peristalsis of the intestinal microflora, enzyme preparations, etc.
Immunosuppressants can be used as monotherapy only in the initial stages of the disease and in the process of diagnosis. Cytostatics in aplastic anemia can be used in combination with immunosuppressants. Also, their important purpose is to purify the concentrate of stem cells from impurities of malignant cells. Antibiotics are used in all stages of the disease to treat concomitant infectious complications that occur against a background of weakened or even absent immunity.
Surgery for aplastic anemia
As pancytopenia progresses, the need for bone marrow transplantation arises - the only radical way to cure aplastic anemia. The problem is that transplantation requires a donor who will provide bone marrow compatible or at least partially compatible in antigenic composition with the bone marrow of the recipient. Finding a donor can take a long time, which in most cases the patient does not have. In such cases, the patient is transfused with whole donor blood or its components in order to maintain a compensated state of his health.In this section, it is necessary to indicate that the operation, as such, is performed only on a bone marrow donor. The recipient is not operated on. In the decades since the first bone marrow transplant in 1968, various methods of introducing stem cells into the body of a patient have been studied. Of all the methods, their intravenous administration proved to be the most effective. It is for this reason that in the future the operation for aplastic anemia will be referred to as stem cell transplantation.
There are the following types of stem cell transplant:
- allogeneic bone marrow transplantation;
- allogeneic transplantation of peripheral blood stem cells;
- autologous cord blood transplantation;
- autologous bone marrow transplantation;
- autologous transplantation of peripheral blood stem cells;
- syngeneic bone marrow transplantation.
Allogeneic bone marrow transplant
This type of treatment involves the extraction of the bone marrow of a donor and its transplantation to a sick recipient. The implementation of this procedure is a technically complex process and implies compliance with certain rules.First of all, the donor must be compatible with the recipient's body for three antigens in two HLA histocompatibility complexes. As a result, complete similarity of the donor and recipient is expected for 6 antigens. The minimum threshold at which transplantation can be performed is a match for 4 out of 6 antigens, however, in this case, the risks of various kinds of complications increase several times. According to rough estimates, only in 30% of cases, among the closest relatives of the patient, donors are found that are fully compatible for all 6 antigens. It doesn't matter the age or gender of the donor. The youngest donor in the world was a four-month-old baby weighing 3.6 kg.
The operation to extract the bone marrow is a modification of the trepanobiopsy with some changes. First of all, this intervention is much more painful, so the use of general or epidural anesthesia is mandatory. The needles used have a large diameter. The puncture is performed 10 to 20 times in the crest of each ilium. The amount of material taken is much higher and amounts to 10-15 ml per kilogram of the donor's body weight. Thus, from a donor weighing 70 kg, an amount of bone marrow equal to 700 - 1050 ml will be taken. Complications after such a procedure develop in less than 1% of cases. The vast majority of complications are associated with anesthesia and acute heart failure with massive blood loss.
Subsequently, the resulting bone marrow is slowly transfused into the recipient's body using intravenous access. However, such cases are quite rare, and more often the bone marrow is obtained from special storage banks of biological materials. These banks are replenished by donors around the world. To date, there are more than 50 national biological storage banks and more than 4 million donors worldwide. After bone marrow is isolated, it must be preserved for a long time. To do this, it is placed in a special solution that does not form ice crystals during freezing and thawing. The cooling rate is 3 degrees per minute. At a temperature of -85 degrees, stem cells are preserved for 6 months. At a temperature of -196 degrees, stem cells are preserved for decades. If necessary, stem cells are thawed at a temperature of 44-45 degrees.
Before the introduction of a suspension of stem cells, they are treated with cytostatics in order to destroy the admixture of malignant cells. For a long period after transplantation, the patient must receive intensive immunosuppressive therapy in order to prevent transplant rejection and other undesirable immune reactions.
Allogeneic transplantation of peripheral blood stem cells
Despite the fact that the above operation is the most common method for obtaining stem cells from a donor's body, in recent years a method for obtaining stem cells from peripheral blood has been actively studied. Its essence lies in the separation of certain types of cells using a physical phenomenon called leukapheresis, followed by blood filtration in special cell separators. In this case, the source of stem cells is donated blood. After extraction, it is enriched with recombinant growth factors, which leads to an acceleration in the rate of division of stem cells and an increase in their number.This method has a number of advantages. Firstly, its side effects are the same as with conventional blood donation. Secondly, the bone marrow of the donor does not suffer, which should be restored during the operation for at least six months. Thirdly, after transplantation of stem cells obtained in this way, adverse immune reactions are less likely to develop.
Autologous cord blood transplant
In some maternity hospitals, in recent years, it has become possible to preserve cord blood extracted from the placenta immediately after childbirth and tying the baby's umbilical cord. Such blood is extremely rich in stem cells. Cord blood is preserved in the same way as described above and stored for many years in biological material storage banks. Blood is stored in case the host develops blood diseases in the future, including aplastic anemia. Stem cells obtained from such blood do not cause graft rejection and are readily available. The disadvantage of such services lies only in the high cost, since the maintenance of a cell in such a bank today is only possible for people with an income much higher than the average level.Autologous bone marrow transplant
This method involves the removal of bone marrow from a patient before a blood disease or at the time of complete clinical remission for the purpose of its further use if necessary. Bone marrow is stored in a similar way. The conflict of incompatibility between donor and recipient stem cells is excluded, since the donor and recipient are the same person.Autologous peripheral blood stem cell transplantation
With this type of transplantation, the patient is transplanted with stem cells extracted from his own blood before the development of a blood disease. The conflict of antigenic incompatibility is also excluded.Syngeneic bone marrow transplant
Stem cell transplantation is performed from a donor who is homozygous ( identical) twin of the patient. The antigens on the surface of the cells of their organisms are identical, so such a transplant will not cause a rejection reaction and is equated to an autologous one.After a stem cell transplant, the patient must be under the vigilant supervision of medical personnel. Active immunosuppressive therapy is mandatory. The patient's low immunity implies his being in specialized sterile wards with a closed ventilation system, bacterial filters, etc. Before entering the ward, medical personnel must be dressed in sterile suits and go through the sanitary inspection room.
Complications of bone marrow transplantation
Complications of bone marrow transplantation are divided into the following groups:- infectious complications;
- graft-versus-host reaction;
- transplant rejection reaction;
- failure of vital organs.
Infectious complications
The development of complications of this kind is typical for both the bone marrow donor and the patient to whom it is transplanted. Suppuration of the postoperative wound in donors develops quite rarely due to the small size of the puncture holes. However, if anaerobic bacteria enter them, there is a risk of developing severe secondary osteomyelitis. Infectious complications in a bone marrow recipient occur due to intense immunosuppression, which is carried out in order to successfully engraft stem cells. Against the background of a decrease in immunity, various bacterial infections join, which must be treated with high doses of broad-spectrum antibiotics.Graft-versus-host reaction
The essence of this complication lies in the conflict of the immune cells of the host organism with the newly formed immune cells of donor stem cells. At the same time, donor lymphocytes show pronounced aggression towards host lymphocytes. Clinically, this is manifested by a profuse rash, skin bullae, ulcers, dysfunction of the gastrointestinal tract, cardiovascular system, etc.This complication develops exclusively when transplanting bone marrow or stem cells from an allogeneic donor. When transplanting your own, previously frozen stem cells, this complication does not develop. This complication occurs when the bone marrow of the donor and the recipient are fully compatible for all 6 antigens in 30% of cases. With partial compatibility, the risk of such a complication increases to 80%. In order to prevent this pathological reaction, cytostatics are used. The most common drug of choice is cyclosporine A in combination with one of the following drugs - methotrexate, imuran, or glucocorticoids ( dexamethasone, methylprednisolone, etc.)
transplant rejection
This complication develops when the host's immune system identifies the donor's stem cells as a threat and seeks to destroy them. It is typical for transplantation of donor stem cells. When transplanting own cells, such a complication is excluded. In patients with aplastic anemia, transplant rejection develops in 20% of cases, that is, in every fifth patient. If this process is suspected, in addition to corticosteroids, recombinant growth factors are prescribed, which increase the rate of tissue fusion.Failure of vital organs
Bone marrow transplantation is a difficult test for all organs and systems of the body. High doses of drugs, in particular cytostatics, have a devastating effect on the tissues of the liver, kidneys, endocrine glands, etc. When the protective reserves of organs are depleted, their functioning stops. The most frequently observed development of acute liver failure and renal failure. The drama of this complication lies in the fact that in most cases the only method of treatment is transplantation of affected organs from donors. But in view of the fact that the cause of organ failure has not been eliminated, it is impossible to transplant a healthy organ, since it will fail in a short time in the same way.Prognosis for aplastic anemia
 The prognosis for aplastic anemia largely depends on the timing of the detection of the disease. With early detection, there is the possibility of more active intervention during the course of the disease. Late detection reduces the chances of a cure.
The prognosis for aplastic anemia largely depends on the timing of the detection of the disease. With early detection, there is the possibility of more active intervention during the course of the disease. Late detection reduces the chances of a cure. Congenital aplastic anemia Fanconi in most cases is extremely difficult to treat, since the bone marrow has never been healthy and, accordingly, it is very difficult to recover. The presence of congenital malformations greatly limits the indications for bone marrow transplantation in such patients. In most cases, patients die in childhood from developmental anomalies or infectious complications.
Acquired aplastic anemias have a more favorable prognosis, since in some cases they are reversible after the cessation of the damaging factor on the bone marrow.
The use of methods of conservation of cord blood, bone marrow stem cells and peripheral blood increases the chances of a full recovery up to 75 - 80%.
Aplastic anemia is more often an acquired acute, subacute or chronic disease of the blood system, which is based on a violation of the hematopoietic function of the bone marrow, namely a sharp decrease in its ability to produce blood cells. This serious disease, even leading to death, fortunately, is rare. The probability of getting sick in men and women is about the same.
Causes of aplastic anemia
Aplastic anemia can develop under the influence of ionizing radiation.Unfortunately, the etiological factors in the development of aplastic anemia in our time are completely unknown. It is believed that these may be:
- regular long-term contact with certain chemicals (benzene and its derivatives, insecticides, etc.);
- ionizing radiation;
- toxic effects on the bone marrow of certain drugs (for example, butadione, indomethacin, some antibiotics - levomecithin, carbenicillin, phenothiazine derivatives - aminazine, diprozine, etmozine, etc.);
- alcohol abuse;
- some infectious diseases (, CMV);
- genetic predisposition.
If the connection with the reasons indicated above cannot be established, aplastic anemia is considered idiopathic.
The mechanism of development of aplastic anemia
As you know, hematopoiesis is provided by a special group of cells - hematopoietic stem cells. They have the ability to multiply and differentiate into various hematopoietic sprouts, from which mature blood cells are subsequently formed - erythrocytes, platelets, leukocytes and others. Under the influence of a number of external or internal factors, the following mechanisms for the development of the disease are possible:
- the number of hematopoietic stem cells in the bone marrow decreases;
- the function of stem cells is disrupted, as a result of which mature blood cells are not formed.
Stem cell damage in this disease is confirmed by the effectiveness of bone marrow transplantation from sisters or brothers compatible in the HLA system or from identical twins. A transplanted bone marrow from an identical twin does not take root in the body of the recipient, unless the latter has previously received a course of drugs that depress the immune system. This fact confirms the immune nature of aplastic anemia.
Signs of the disease
Clinical manifestations of aplastic anemia are very typical. The disease usually debuts acutely. There are 3 characteristic syndromes that indicate the inhibition of one or another hematopoietic sprouts:
- anemic (is a sign of a violation of the formation of red blood cells; patients complain of general weakness, lethargy, drowsiness, irritability, fatigue, poor sleep and appetite, dizziness, tinnitus, palpitations, pallor of the skin);
- hemorrhagic (a sign of reduced platelet count in the blood; pinpoint hemorrhages (petechiae) and hematomas on the skin, frequent nasal and gingival bleeding, heavy periods in women, the presence of blood in the urine, prolonged bleeding even with the slightest cuts, etc.);
- leukocytopenia syndrome (a sign of a reduced content of leukocytes in the blood, in particular neutrophils; frequent infectious diseases that occur for a long time and with complications, chronic foci of infection on the skin, in the lungs and other organs, at first glance, an unreasonable increase in body temperature).
With auscultation (listening) of the heart, the doctor will determine the presence of noise, with palpation (palpation) and percussion (tapping) of the abdomen - an increase and / or. The disease proceeds in different ways: in some cases it progresses quickly, leading to death in several months or even weeks, in others it goes on for a long time, with alternating periods of exacerbations and remissions.
Diagnosis of aplastic anemia
 The most common general blood test will help to identify the disease.
The most common general blood test will help to identify the disease. The results of the simplest examination - a general blood test, in which the number of blood cells - erythrocytes and hemoglobin, leukocytes, platelets, and ESR will be sharply increased, will help to suspect this disease. The degree of decrease in the content of certain elements in the blood is variable in different patients. Changes can coexist in isolation or in parallel. There may be a predominance of the number of one class of cells over another. To confirm the diagnosis, a bone marrow biopsy is necessary: a special needle is used to pierce the sternum or ilium, penetrate into the bone marrow and take some of it for examination. Microscopically, in aplastic anemia, the predominance of adipose tissue cells in the bone marrow, in which there are slight inclusions of individual islets of hematopoietic cells, is determined. Based on the data of a general blood test and the results of a myelogram, experts have proposed criteria for making a diagnosis of a severe form of aplastic anemia:
- in peripheral blood - the number of neutrophils is less than 0.5 * 10 9 / l, platelets - less than 20 * 10 9 / l, reticulocytes - less than 20 * 10 9 / l;
- in the bone marrow - the content of myeloid cells is less than 25%.
Treatment of aplastic anemia
Treatment of this disease includes 3 components: etiological, pathogenetic and symptomatic. If the causes that could cause anemia are known (for example, prolonged contact with insecticides), it is necessary to eliminate them as soon as possible - it is very likely that the hematopoietic function will then normalize. Since anemia, which is a mandatory symptom of the disease, leads to serious disturbances in microcirculation in organs and tissues and to their oxygen starvation, it is necessary to strive to normalize this link: the patient is prescribed red blood cell transfusions, while striving for a hemoglobin value of 80 g / l. Bleeding is the leading cause of death in people with aplastic anemia. To eliminate, the patient should be prescribed platelet concentrates - thrombus mass. In addition, in order not to provoke bleeding, physical activity is not recommended for patients, aspirin and other anti-inflammatory drugs are prohibited, and women should take drugs that inhibit (suppress) ovulation.
A reduced number of leukocytes and neutrophils - leukopenia and neutropenia - are the third hematological sign of aplastic anemia. It is impossible to correct the level of these elements in the blood by transfusions of leukocyte suspensions, since they circulate in the body for only a few hours and then die. In this situation, preventive measures and timely treatment of infectious diseases come to the fore. For this purpose, antibacterial (Norfloxacin), antiviral (Acyclovir) and antifungal (Fluconazole) drugs can be prescribed. If, against the background of this therapy, the patient's body temperature does not normalize, drugs that stimulate hematopoiesis are recommended. In the case when there is no effect from this drug, the patient may be prescribed infusions of granulocytes. To restore the hematopoietic function of the bone marrow, several groups of drugs are used.
- Corticosteroids, or steroid hormones. They can be prescribed only in combination with other drugs, they are not used in isolation, since the risk of infectious complications increases against the background of their use.
- Androgens. Widely used in the treatment of aplastic anemia. The effect of these drugs depends on the severity of the disease. To achieve a positive result, a long-term continuous intake of androgens is required - for several months and years. As a result of their intake, the frequency of blood transfusions decreases, and the quality of life of patients improves. Side effects are virilization (appearance of masculine features (hairiness, rough voice) in women).
- Cytokines (CSF-GM). The use of these drugs can partially correct cytopenia only if the residual hematopoietic function is not lost (i.e., the bone marrow works, but very weakly). A greater effect of cytokines is noted after bone marrow transplantation and the use of drugs that depress the immune system.
- Immunosuppressors (drugs that depress the immune system: Cyclophosphamide, Cyclosporine, etc.). The use of these drugs sometimes even leads to a complete restoration of the function of hematopoiesis.
The most effective treatment for idiopathic aplastic anemia is BMT - bone marrow transplantation. The ideal option is the bone marrow of the patient's identical twin. In this case, the survival rate is about 80-86%. The younger the recipient, the higher his chances of a 5-year survival after BMT. However, even after complete restoration of the hematopoietic function, a recurrence of the disease is possible after 5 years.
Forecast
The prognosis of aplastic anemia depends on many factors, the main of which are:
- the degree of inhibition of the hematopoietic function of the bone marrow;
- patient's age;
- the nature and tolerability of the treatment to patients.
In persons under 30 years of age, the prognosis is more favorable, but in the case of severe and super-severe forms of the disease, it is more pessimistic. If the patient receives only symptomatic therapy, the probability of surviving 1 year is only 10%. With the use of pathogenetic therapy, and even more so with BMT, the life expectancy of people suffering from aplastic anemia increases many times over. In some cases, a complete recovery is possible.
Aplastic anemia is the rarest of all major drug-induced hematological disorders, but has the highest mortality rate. Its frequency rises sharply among people over 65 years of age, in women this complication occurs more often than in men [Bodir et al., 1979].
Clinical manifestations
The clinical picture of drug-induced aplastic anemia is highly variable. Usually, aplasia develops 4-8 weeks later, and sometimes more, after exposure to the drug. As a rule, it occurs after repeated exposure to the drug, which indicates the immunological mechanisms of damage. In the elderly, the onset may be sudden with bleeding or infection, but it usually develops gradually, with symptoms of anemia such as weakness, fatigue, and shortness of breath. Sometimes the infection manifests itself in the form of toxicosis with phenomena of confusion. Bleeding may be minor, but sometimes it is so severe that it causes fatal brain hemorrhages. Examination of the patient reveals signs of anemia, infection and thrombocytopenia. Slow progression of symptoms can make it difficult to obtain an accurate history of drug use; reliable data can be obtained only in about 40% of patients.
Blood and bone marrow changes
Aplastic anemia is characterized by a normocytic or macrocytic (mild to moderate) picture of peripheral blood, while two of the following three signs are found: the number of granulocytes falls below 0.5-109 / l, the number of platelets is below 20-109 / l, the content reticulocytes is less than 1%. With the gradual development of symptoms, the hemoglobin level is usually less than 70 g / l. Neutrophils may show toxic granularity and increased alkaline phosphatase activity. Immature leukocytes and normoblasts appear in the peripheral blood. With moderate leukopenia, only the content of neutrophils decreases, but in severe cases, lymphopenia and monocytopenia are observed. In bone marrow trepanates, in typical cases, along with reduced cellularity, foci of normal or increased cellularity are detected. ESR is accelerated. Studies with 59Fe reveal a decrease in iron clearance and turnover, a decrease in iron uptake by the bone marrow, its low utilization, and the absence of foci of extramedullary hematopoiesis. When cultivating bone marrow in agar, few colonies are formed, but their growth is not disturbed.
Drugs that cause aplastic anemia
Aplastic anemia can be caused by a variety of drugs, but most cases are due to relatively few drugs. Bottiger et al. (ShZh) reported a significant recent change in the spectrum of substances that cause aplastic anemia: if in 1966-1970. oxyphenbutazone, levomycetin and butadion most often appeared in the messages, then in 1971-1975. - sulfonamides, cytostatics and diacarb. However, Timoney (1978) found that butadione and oxyphenbutazone were still the most frequently reported in reports sent to the WHO Research Center in 1968-1975.
The drugs that cause aplasia are described below, and first of all those that are usually prescribed to elderly patients.
Antibacterial agents
Levomycetin. This drug has a dual effect on the bone marrow. It most commonly causes reversible, dose-dependent bone marrow suppression, predominantly affecting erythroid cells and sometimes also platelets and granulocytes. Less commonly, irreversible, late onset bone marrow aplasia develops, involving all three cell lines and accompanied by high mortality.
Knowledge of the danger of these complications has led to a sharp reduction in oral and parenteral use of chloramphenicol. However, cases of aplasia were also noted after local use of chloramphenicol in the form of an aerosol or its use as part of eye ointments. Although none of the patients were elderly, these observations highlight the need for caution in the use of such topical agents. It is not clear how a systemic effect develops when applied topically. It can be assumed that it is a consequence of the absorption of substances through the conjunctiva or its entry through the lacrimal duct into the gastrointestinal tract.
Sulfonamides, penicillins and metronidazole. These drugs sometimes cause aplasia, including in the elderly (White et al., 1980).
Medicines used to treat rheumatic diseases
Butadione and oxyphenbutazone. McCarthy, Chalmers (1964), having analyzed the relationship of butadione with bone marrow aplasia, found that most cases occur in women over 60 years of age. These patients, as a rule, did not take other drugs that could cause aplasia. Later, Fowler (1967) concluded that butadione and oxyphene-butazone in young patients most often cause agranulocytosis, and in the elderly - aplastic anemia. Mortality increases sharply with age, symptoms of the lesion develop after a few months from the start of treatment. Inman (1977) analyzed the medical records of 269 patients whose death certificates did not mention drugs as the cause of aplasia or agranulocytosis. He found that 83 deaths (31%) were likely drug-related, with 128 deaths due to butadione and 11 to oxyphenbutazone. And in these cases, mortality increased sharply with age, especially among older women. Excessive mortality in this particular age group is not associated by the author either with the high use of drugs, or with the fact that women live longer than men.
Preparations of gold. The relationship between bone marrow aplasia and gold supplementation was studied by Kau (1973, 1976). In most patients, bone marrow depression developed after taking 450 mg of gold, but in some cases a lower dose was sufficient. Eosinophilia, traditionally regarded as an alarming symptom, has been found in only a few cases. This may be partly due to the fact that in such patients the leukocyte formula was counted irregularly. Cow concluded that aplasia is a serious but rare complication of gold therapy and that the best ways to prevent it are regular complete blood counts and dose reduction when clinical remission is achieved.
D-Penicillamine. With prolonged use, it can cause a decrease in the number of red blood cells, neutrophils and platelets. Kau (1979), when describing 10 patients with pancytopenia caused by penicillamine, noted that the dose of the drug varied from 250 to 1000 mg/day, averaging 615 mg/day. The duration of treatment was 3-60 months, on average - 10 months. The age of the patients ranged from 35 to 68 years. Opinions about the role of penicillamine in the development of aplasia in individuals who have previously received gold preparations are contradictory. Smith, Swinburn (1980) on the basis of personal experience believe that in patients who have previously undergone adverse reactions to gold preparations, the frequency of adverse reactions to penicillamine does not increase, and that the risk of developing such reactions does not increase when starting penicillamine therapy for 6 months after discontinuation of treatment with gold preparations. However, Keap et al. (1980) believe that the likelihood of developing reactions to penicillamine is higher in patients who have had previous reactions to gold preparations.
Other anti-inflammatory drugs that may be associated with the development of aplasia include indomethacin, sulindac, and fenprofen.
Cytotoxic agents
These drugs, in full accordance with their nature, suppress the functions of the bone marrow, so they are usually prescribed in the form of intermittent courses. This group of drugs includes alkylating agents such as cyclophosphamide, myelosan and melfan; antimetabolites such as methotrexate and mercaptopurine; vinca alkaloids, including vincristine and vinblastine.
Anticonvulsants
Hydantoin derivatives can cause aplasia. Ni-guley et al. (1966) noted that, according to the registry of the American Medical Association, out of 50 cases of aplasia associated with taking anticonvulsants, 45 were caused by diphenine and methylphenylethylhydantoin. Gabriel et al. (1966) described 16 cases of aplasia caused by hydantoin derivatives. The age of the patients was 9-48 years, most of them were men. According to the same authors, patients with aplasia caused by oxazolidine derivatives also belonged to the same age group.
The association of carbamazepine with aplasia was analyzed by Hart, Easton (1981) . They concluded that the incidence of such cases is less than 1:50,000. The duration of therapy before the development of aplasia ranged from 4 to 330 days. The age of the patient and the total dose of the drug were not among the important causal factors determining the development of aplasia. The authors believe that routine laboratory monitoring of the condition of patients is not justified.
Antidepressants
Mianserin was the subject of a report in Current Problem in 1983. This drug causes severe blood disorders including aplastic anemia. The frequency of hematological disorders in 1982 was about 3 cases per 100,000 patients who took this drug. The mean age of the patients was 67 years. The number of cases of aplasia in the elderly was higher than what could be expected given the more frequent use of the drug in this age group. Durrant, Read (1982) described a fatal outcome in a 65-year-old woman.
Antithyroid drugs
Thiouracil, due to its associated toxic effects, including aplasia, is currently little used. Carbimazole is less toxic, but it sometimes causes aplasia in elderly patients.
Other medicines
Oral antidiabetic drugs such as chlorpropamide and butamide can rarely cause aplasia in middle-aged patients. Aplasia caused by chlorpropamide develops within 1 month from the start of treatment or after 6 months - 7 years. Cimetidine usually causes agranulocytosis, but a case of aplastic anemia has been described in a 49-year-old woman who took this drug along with a large number of other drugs, including paracetamol, which itself can cause aplasia.
Hematopoietic stimulants are drugs that stimulate the bone marrow, increasing the production of erythrocyte, leukocyte sprouts together or separately. Also, such drugs intensify the differentiation of blood cells and accelerate the maturation of young forms of blood cells and their transformation into mature erythrocytes or leukocytes. Such drugs are used in many cases when natural hematopoiesis is suppressed for some reason: radiation injuries, the consequences of chemotherapy or radiotherapy of oncopathologies and systemic diseases, chronic renal failure against the background of various kidney pathologies, rheumatoid arthritis, acute or chronic infectious processes, myeloid leukemia .
Medicines of this group should be used only after establishing a diagnosis confirmed by additional studies. Self-administration is inappropriate and unsafe.
Medications to stimulate hematopoiesis
I. Erythropoiesis stimulants not only increase the production of red blood cells, but also accelerate their maturation, make them more stable, able to move in the vessels, increase their saturation with hemoglobin. Described in detail in the section “Treatment of anemia”.
1. .
A) divalent iron. Ferroplex, sorbifer durules, tardiferron, ferrogradumet, gynotardiferron, ferretab, fenyuls, actiferrin, totem, hemofer, hematogen.
B) trivalent iron. Maltofer, fenyuls, ferrum lek, ferlatum.
For parenteral administration: venofer, maltofer, ferrum lek, argeferr, kosmofer, likferr.
2. : B12 (cyanocobalamin), folic acid, ascorbic acid, vitamins E, B2, B6.
3. nandrolone, mesterolone, anapolone (oxymetholone).
4. testosterone propionate, sustanon.
5. . Epoitin alfa (Eralfon, Epocomb, Eprex, Epokrin, Repoetir-SP). Epoitin beta (vero-epoitin, epostim, epoitin-vero, erythrostim, erythropoietin, recormon). Epoitin omega (epomax). Darbepoitin alfa (aranesp).
II. Leukopoiesis stimulants. They are used for depressions of the granulocytic germ, with the exception of blood tumors. Effective for the consequences of treatment with cytostatics, radiation therapy, radiation sickness, a decrease in leukocytes against the background of chronic infections, human immunodeficiency syndrome and oncopathologies. Stimulate the bone marrow and lymphoid tissue with neutropenia and agranulocytosis.
1. needed for stimulation and differentiation of the granulocyte-monocyte colony-forming unit, from which eosinophils, monocytes and neutrophils are formed. According to the chemical structure, these are glycoproteins involved in the production of macrophages, megakaryocytes, granulocytes. They enhance the release of granulocytes from the bone marrow into the blood, activate phagocytic activity. Increase the cytotoxicity of mature granulocytes.
Granocyte, lenograstim (recombinant human granulocyte colony stimulating factor) lyophilisate, dicarbamine tablets, grasalva injection, neupogen (filgrastim), neipomax, neulastim (pegfilgrastim), tevagrastim, zarcio.
2. . The drug thiazolidine decarboxylic acid, stimulating leukopoiesis. Contraindications are leukemia and lymphogranulomatosis.
3. . Sodium nucleinate. Sodium deoxyribonucleate. Sodium salts obtained from the hydrolysis of yeast fungi. In addition to stimulating leukopoiesis, it activates macrophages, thereby enhancing phagocytosis. Stimulate T and B lymphocytes. In powder for solution for injection and in tablets.
4. . Methyluracil, pentoxyl tablets. They combine the properties of a leukopoiesis stimulator with a regenerating function.
5. . Interleukin-1 beta (betaleukin). The drug potentiates the release of colony-stimulating factors by other cells, for example, the endothelium of the vascular wall. The result is a more rapid maturation of leukocytes and their release into the bloodstream from the bone marrow.
Drugs that stimulate hematopoiesis should be prescribed according to strict indications by a hematologist. With self-medication, numerous severe consequences of uncontrolled use of such drugs are possible.